Diabetic Gastroparesis
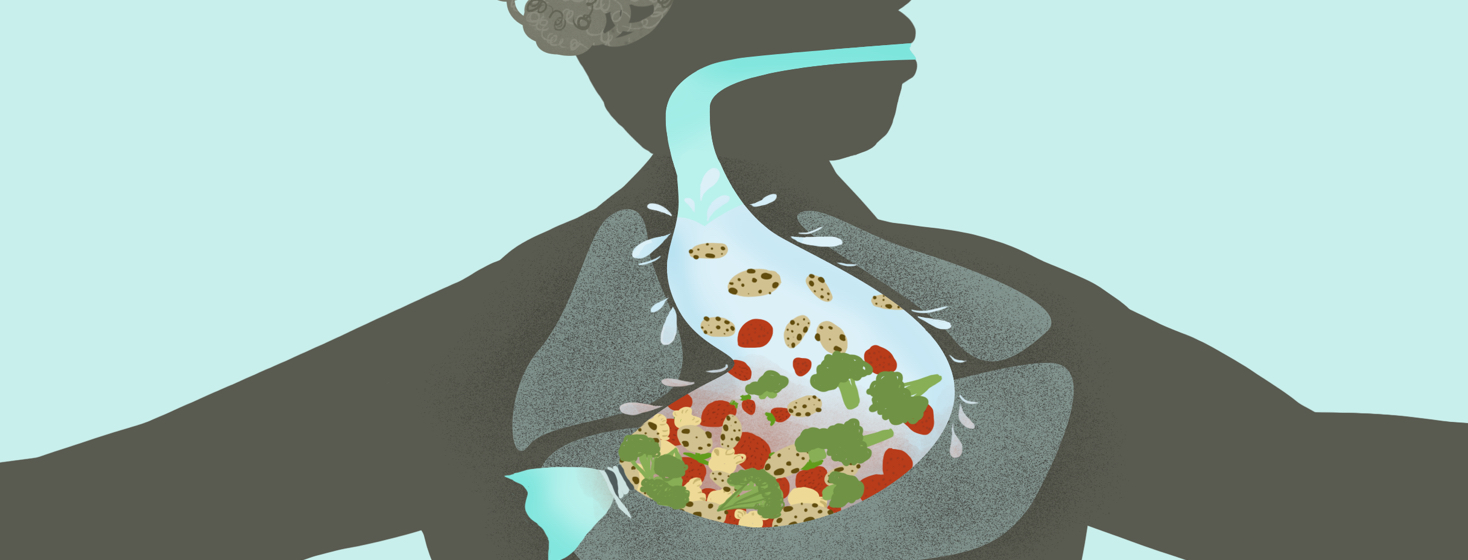
Gastroparesis, also known as delayed gastric emptying, is a digestive condition that affects the way the stomach moves food through the intestines. Muscular contractions in the stomach help break down the food you eat and move it through the digestive tract. Gastroparesis interferes with normal spontaneous movement (motility) causing the stomach to slow down, and interrupt digestion, thereby preventing the stomach from properly emptying.
Gastroparesis and type 2 diabetes
Gastroparesis can affect anyone but is common in people with type 1 and type 2 diabetes. For diabetics, neuropathy is a common complication. Neuropathy can occur when there is damage to the peripheral nervous system, the communications network that sends signals between the brain and spinal cord to other parts of the body.
Elevated blood glucose levels over a prolonged period may result in chemical changes to the nerves resulting in damage to the blood vessels which oxygenate and fuel the nerves. The vagus nerve controls contractions in the stomach and the intestines. When it is damaged, the signals that tell the muscles to move the food through the steps of digestion don’t work right and the process slows down or stops.2,3 This leaves the food sitting in your stomach longer. 1
Gastroparesis can make it more difficult for a diabetic to manage their blood sugar levels.1 When digestion is disrupted, delayed absorption of nutrients you eat can sometimes make it unpredictable to manage when to take insulin.1 This can cause a dramatic fluctuation in blood sugar levels.
Symptoms of gastroparesis
Symptoms of gastroparesis will vary, with some having mild or severe symptoms and others having none. Signs and symptoms include:2,3,4
- Heartburn
- Nausea and Vomiting, usually of undigested food
- Feeling of fullness after minimal eating
- Weight loss
- Abdominal bloating
- Unstable blood glucose (sugar) levels
- Lack of appetite and unintentional weight loss
- Gastroesophageal reflux (GERD)
- Stomach spasms
Additional complications from gastroparesis
Food that stays in the stomach too long can ferment and cause bacterial overgrowth. It can harden into solid masses, called bezoars, that can bring on feelings of nausea, and trigger vomiting or stomach obstruction. Bezoars are indigestible and can be dangerous when they block the small intestine. When the food eventually passes through the small intestine where it is absorbed, it causes blood glucose levels to rise.3 Other concerns include severe dehydration, malnutrition, and a disruption to quality of life.4
Diagnostic tests for gastroparesis
There are a number of testing options to evaluate gastroparesis.2,3
- Barium X-ray after fasting for 12 hours, drink a liquid that contains barium followed by an abdominal X-ray to see if there is still food remaining in the stomach.
- Barium Beefsteak Meal Eat food that contains barium followed by imaging tests so doctors can observe how the meal digests and how long it takes for food to leave.
- Radioisotope gastric Emptying Scan Eat food that contains a radioactive compound followed by imaging tests.
- Gastric Manometry Measures stomach muscle activity. It is a narrow tube placed through the throat to the stomach which includes a device to measure the stomach's activity as it digests food.
- Blood tests check for nutritional deficiencies and electrolyte imbalances.
- Upper endoscopy checks for abnormalities in the structure of the stomach.
- Ultrasound can be used to measure the rate of emptying a liquid meal by repeated evaluation of cross-sectional changes in volume. Also rules out other abdominal diseases. Sound waves outline and define the shape of the gallbladder and pancreas.
Treatment for gastroparesis
Treatment options include one or more of the following:3
Insulin adjustments
Changing the dosage and timing of insulin can help to better manage blood sugar levels. Guided by your physician you may be advised to:
- Use insulin more often
- Take insulin after eating rather than before
- Check blood glucose levels more frequently after eating to accommodate any delayed rise in blood glucose
Oral medications include drugs that stimulate stomach muscles and reduce nausea. Avoid any drugs that delay gastric emptying like opiates.
Dietary changes
Eating frequent smaller meals (grazing) can help manage symptoms of gastroparesis. A doctor or nutritionist can tailor specific advice to improve your symptoms. General tips include: 2,3
- Reduce or avoid eating high-fat and high-fiber foods. They can take longer or be more difficult to digest and can increase symptoms.
- Eat more slowly, stay upright after meals, and try taking a walk.
Some diabetics with gastroparesis require surgery to insert a feeding tube, also called a jejunostomy tube. This permits the nutrients to do directly into the small intestine, bypassing the stomach. Others may get IV nutrition if gastroparesis is very severe, resulting in malnutrition or severe difficulty managing blood glucose levels.
Importance of good management
Gastroparesis can lead to more frequent hospitalizations and ER visits for people with diabetes. They may also experience damage to the eyes or kidneys, an increased risk for heart disease, and other complications compared with diabetics who do not experience gastroparesis.2 This can increase the risk of early death due to diabetes-related causes. 2
Gastroparesis is a chronic condition, not cured by available treatment. However, managing gastroparesis with treatments, including lifestyle changes, can help maintain a good quality of life.3
Join the conversation